Understanding the Unique Mental Health Challenges Faced by Veterans
Veterans often navigate a complex and unique set of
mental health challenges, including depression, post their military service. The transition from a highly structured, mission-focused life to a less defined civilian existence can be disconcerting. This transition is often marked by a loss of identity, a sense of purposelessness and feelings of isolation, which can contribute to depression. Adding to the complexity, veterans often face tangible triggers such as physical injuries and invisible triggers like post traumatic stress disorder (PTSD), which can exacerbate their mental health issues.
At the same time, specific experiences during their service, such as exposure to combat or traumatic events, substantially increase the risk for conditions like depression, anxiety and
PTSD. The ingrained military culture of self-reliance and stigma associated with seeking help further augments their challenges. Thus, understanding the unique mental health challenges faced by veterans, demands acknowledgement of both the macro factors like transition struggles and micro factors like individual traumatic experiences.
Assessing the Prevalence of Depression Among Veterans
The analyses of several studies reveal a startling reality: our veterans are grappling with higher rates of depression than the rest of the population. According to the
Substance Abuse and Mental Health Services Administration (SAMHSA), approximately 3.7 million veterans dealt with a mental health issue in 2018, a large proportion of which included
depression. The Verywell Mind reports that up to 30% of veterans returning from the Middle East conflicts are diagnosed with a depressive disorder, an estimate 2 to 5 times higher than the prevalence within the general American population.
Further research underlines the grave severity of the situation. In a study published by U.S. Veterans Affairs, amongst veterans who fought in Iraq and Afghanistan, 13.5% were diagnosed with depression. Furthermore, the National Alliance on Mental Illness (NAMI) states that out of 20 veterans that commit suicide each day, many suffer from untreated or under-treated depressive illnesses. For women veterans, the prevalence of depression is higher than their male counterparts, as they are twice as likely to suffer from depression or post-traumatic stress disorder (PTSD). These statistics demonstrate a public health crisis among veterans that needs urgent attention.
The Correlation Between Military Service and Depression
Military service inherently involves exposure to unique and often challenging circumstances. Veterans, in their tenure, have had experiences that range from rigorous training and deployment related stress to, in some cases, direct combat exposure. These situations can incite a variety of stress reactions, increased anxiety levels and even trigger more intense mental health conditions. One such condition that exhibits extensive prevalence among the veteran community is depression.
Clinical evaluations and studies consistently indicate a significant relationship between military service and the advent of depressive symptoms. Furthermore, this correlation appears more pronounced among service members who have experienced combat. This complex mental health challenge often stems from the after-effects of traumatic experiences, brutal confrontations, and an overall high-stress environment that military personnel commonly encounter. Consequently, the need for specialized mental health services catering to the depression-related needs of veterans becomes increasingly critical.
Mental Health Resources Available for Veterans in Middletown Township
In the dedicated pursuit of better health outcomes, Middletown Township offers a myriad of mental health resources for servicemen and servicewomen. Veterans can avail themselves of professional counselling services, group therapy sessions, and psychiatric treatment programs. The aim of these facilities is to nurture a healing environment which employs a comprehensive approach towards addressing the unique mental health challenges faced by veterans.
Moreover, an emphasis is placed on psychological resilience and self-management skills. The regional VA Middletown Health Care System, private clinics, and non-profit organizations work collaboratively to deliver these services. They deliver specialized treatments and employ a cadre of healthcare professionals well-versed in the intricacies of post-service mental health conditions, including depression. These resources form an integral component of the comprehensive care needed to effectively navigate the path towards improved mental health.
The Importance of Specialized Treatment for Veterans Suffering from Depression
Veterans suffering from
depression require specialized treatment approaches that are designed to cater to their unique experiences and needs. This importance is underscored by research indicating veterans as having twice the likelihood of suffering depression as compared to the general population. This high prevalence is often linked to varied causes such as Post Traumatic Stress Disorder, experience in combat zones, and the stress of reintegration into civilian life. Each of these causes dramatically shapes their struggles with depression, underscoring the imperative to have targeted therapeutic interventions and treatments.
Without specialized treatment, the unique mental health challenges faced by veterans may be overlooked or inadequately addressed. Qualified mental health practitioners proficient in veteran-specific therapy techniques are well-equipped to guide these brave individuals on a meaningful path to recovery. Moreover, specialized treatment plans tend to incorporate holistic approaches, addressing these veterans’ realities such as concomitant physical health issues, potential substance misuse, and social reintegration challenges. Overall, specialized treatment, in its understanding and accommodation of this group’s unique circumstances, reigns paramount in addressing the prevalent issue of depression among veterans.
How to Recognize Signs of Depression in Veterans
Depression might show itself in a multitude of different ways among veterans. The symptoms may be physical, emotional, or changes in the way that persons think or behave. Frequently reported symptoms include a loss of interest in previously enjoyed activities, feelings of hopelessness, irritability or restlessness, difficulties sleeping or concentrating. More drastic signs might also include expressions of death or suicidal thoughts.
Recognizing depression in veterans does not necessarily require a professional role as it heavily relies on observing changes in a person’s behaviour or listening to what they communicate. However, the stigma associated with mental health can often create a barrier for veterans to disclose their struggles. Therefore, it becomes crucial for those around them – family, friends, and military personnel to stay vigilant for any behavioral changes underscoring depression, ensuring timely intervention.
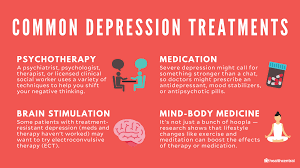
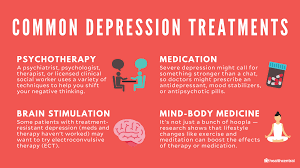
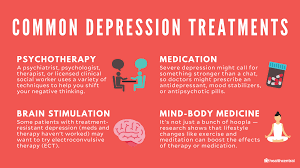
Approaches to Depression Treatment for Veterans
Depression, a common mental health challenge among veterans, necessitates specialized treatment approaches. These approaches often emphasize a combination of psychotherapy, medication, and supportive aid tailored to suit the needs of each individual. Psychotherapy, particularly cognitive behavioral therapy, has shown efficacy in managing depressive symptoms by enabling veterans to understand and modify their thought patterns. Medications like antidepressants can also be beneficial in managing these symptoms, however, they are often most effective when utilized in conjunction with therapy.
In addition to these traditional techniques, innovative treatment approaches for veterans battling depression are continually evolving. This includes virtual reality exposure therapy, which can assist in processing traumatic experiences from the battlefield. Another prevailing approach is the use of peer support groups, where veterans can share experiences and coping strategies in a supporting and understanding environment. These shared experiences often provide reassurance, reducing feelings of isolation commonly associated with depression. Clear and consistent communication between veterans, their healthcare providers, and their support networks is crucial in customizing and implementing the most effective treatment plan.
The Role of Support Systems in Mental Health Treatment for Veterans
Support systems play a crucial part in the mental health treatment of veterans, offering comprehensive help that extends beyond the clinical approaches. These systems can involve close family members, friends, professional consultants, therapists, and veteran peer networks. They offer comfort, affirmations, guidance, and a sense of comradeship, which is especially crucial for combat veterans. Such systems counter feelings of alienation and misunderstanding by bridging the gap between the veteran’s experience and civilian life. They play a unique role in fostering a sense of belonging and acceptance that bolsters their emotional resilience, thereby aiding the process of healing.
In addition to emotional support, these systems also prove invaluable in providing care management services and navigating complex healthcare bureaucracies. Professionals embedded within these systems render assistance with tasks such as scheduling and attending medical appointments, medication management, filing paperwork, and understanding treatment plans. By providing these support services, these networks help veterans focus more on their recovery instead of administrative burdens, thereby ensuring a smoother process of mental health treatment. In a nutshell, support systems function as an invaluable adjunct to therapy in mental health management for veterans.
Success Stories: Veterans Overcoming Depression in Middletown Township
In
Middletown Township, a myriad of veterans have effectively battled and triumphed over depression, demonstrating resilience and courage that undoubtedly constitute a beacon of hope. Take the case of Henry, a war veteran who dealt with severe depressive bouts for years after returning from service. After years of denial and resistance, he was persuaded to seek professional help. With dedicated treatment, which included cognitive behavioral therapy and medication, and the continuous backing of a solid support system, Henry managed to turn his life around. He is now an advocate for mental health among his peers, willingly sharing his journey to encourage others in similar situations to seek help.
In a likewise inspiring account, there is Sarah, another veteran who carried her war nightmares, manifested as depression, into her civilian life. This condition punctuated her daily life until a veteran support group in the town suggested she attend therapy sessions offered by a local mental health organization. One year into her therapy, Sarah showed significant improvement and now leads a balanced, fulfilled life. She has taken this one step further by training as a mental health nurse and offering help to veterans who also struggle with depression. These success stories highlight the impact and immense value of mental health support systems in the recovery journey of depressed veterans.
Future Directions for Improving Mental Health Services for Veterans
The call for further augmentation of mental health services for veterans is imperative. Central to this conversation is the importance of establishing more specialized approaches that will help curb the rising cases of mental health maladies amongst this specific group. Embracing innovative tactics such as personalized mental health interventions can offer a pathway towards addressing some of the unique psychological challenges that veterans face. Through such strategies, not only will mental health service delivery be enhanced, but veterans’ overall well-being will be vastly improved.
In addition, there is a pressing need to incorporate technological advancements in the realm of mental health, particularly Telepsychiatry. This digital means of delivering psychotherapeutic services will play an instrumental role in reaching out to even the most secluded of veterans. It can facilitate access to mental health services, especially in the face of geographic constraints, thus bridging the gap in service delivery. Ultimately, a comprehensive and forward-looking approach that incorporates draconian strategies alongside modern techniques will be instrumental in improving mental health services for veterans.