Exploring the Relationship of Sleep and Depression
Sleep and
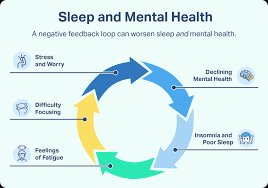
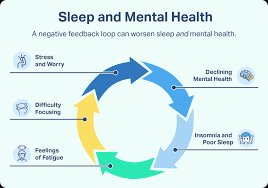
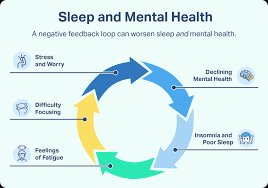
depression hold an intricate relationship, interwoven in ways that often make it challenging to distinguish cause and effect. Researchers have observed that individuals suffering from depression frequently experience sleep problems; these may range from insomnia, characterized by difficulty in falling or staying asleep, to hypersomnia, characterized by excessive sleepiness. Interesting to note is that not only is sleep disruption a common symptom of depression, but persistent sleep issues can also increase the likelihood of developing or exacerbating depressive disorders.
Conversely, optimizing sleep patterns can help improve mood and act as a protective factor against depression. A well-regulated sleep cycle promotes emotional stability, cognitive function, and overall well-being. It becomes a self-reinforcing cycle – sound sleep lessens depressive symptoms, and lower levels of depressive symptoms lead to better sleep quality. However, it is crucial to remember that this is a complex relationship and manipulating sleep alone is not a singular cure for depression. Other factors and comorbid conditions significantly contribute to both sleep quality and depression severity.
Unpacking the Concept of Sleep Disorders
Sleep disorders are a broad category of conditions that affect how well and how much one sleeps. These conditions are clinically distressing or impair one’s daily functioning, with issues ranging from initiating sleep, maintaining sleep, to experiencing non-restorative sleep or excessive sleepiness. According to the American Academy of Sleep Medicine, sleep disorders have been classified into six main categories – Insomnia, Sleep related breathing disorders, Central disorders of hypersomnolence, Circadian rhythm sleep-wake disorders, Parasomnia and Sleep related movement disorders. Each of these present a unique blend of symptoms, resulting in a specific diagnosis.
For instance, insomnia, arguably the most recognized sleep disorder, is characterized by persistent difficulties with falling asleep, staying asleep, or waking up too early and being unable to return to sleep. On the other hand, circadian rhythm sleep-wake disorders relate to disruptions in the body’s internal clock leading to mistimed sleep and wake periods. Parasomnias manifest through undesired events occurring just before sleep onset, during sleep, or around wake-up times, such as sleepwalking, sleep talking, or nightmares, while sleep related movement disorders involve simple, repetitive movement during sleep, such as restless leg syndrome. Understanding the diverse nature and the intricacies of these sleep disorders is a fundamental step towards devising suitable therapeutic strategies.
Depression: A Brief Overview
Depression, classified as a mood disorder, is characterized by a pervasive and persistent low mood accompanied by a significant decline in interest or pleasure in activities that were once enjoyable. The condition has a variety of symptoms such as feelings of guilt or worthlessness, fatigue, difficulty concentrating, and at its worst, suicidal ideation. The nature and severity of symptoms vary widely among individuals, but one certainty is the substantial and detrimental impact that depression has on an individual’s overall well-being and ability to function.
The prevalence of depression has grown exponentially, with the
World Health Organization identifying it as one of the leading causes of disability worldwide. While genetic predisposition seems to be a significant risk factor for depression, environmental factors such as stressful life events, physical illnesses, and adverse childhood experiences potentiate its occurrence. Researchers have also identified altered neuroendocrine function, mainly involving the hypothalamic-pituitary-adrenal (HPA) axis, as a critical physiological mechanism underlying depression.
The Bi-directional Link between Sleep and Depression
Emerging research illustrates a profound interconnectedness between sleep disturbances and depression implying a complex, bi-directional relationship. Those suffering from depression often report insufficient sleep or sleeping excessively, while individuals with insomnia or sleep disorders have a higher probability of developing depression compared to those without. This demonstrates that the relationship between sleep and depression is not merely correlative but interactive and symbiotic.
The biological influences underpinning this reciprocal relationship include disruptions in the circadian rhythm and altered
REM (rapid eye movement) sleep. The circadian rhythm, our body’s innate 24-hour cycle that helps regulate sleep and wakefulness, may be disrupted in individuals with depression. Similarly, people with depression often experience irregularities in REM sleep, which can lead to decreased sleep quality. In turn, poor sleep can exacerbate depressive symptoms, fueling a debilitating cycle. This foundational understanding drives the need for comprehensive treatment strategies that target both sleep disturbances and depressive symptoms.
How Poor Sleep Quality Influences Depression
Disruptions in sleep patterns can significantly impact an individual’s overall well-being and predispose them to depressive symptoms, encompassing both cognitive and affective domains. For instance, poor sleep latency (the time it takes to transition from complete wakefulness to sleep), frequent awakenings throughout the night, and poor sleep efficiency (the total time spent sleeping divided by the total time spent in bed) can trigger emotional dysregulation. This dysregulation can lead to cognitive deficits, such as impaired memory and concentration, which can initiate and perpetuate depressive symptoms.
Moreover, the link between sleep disturbances and depression may be underlined by common neurobiological pathways involving dysfunctions in neurotransmitters, such as serotonin, gamma-aminobutyric acid (GABA), and dopamine. Disruption of these neurotransmitters subsequently results in the imbalance of the brain’s emotional circuitry, thereby leading to depression. Empirical findings illustrate that reduced slow-wave sleep (SWS), or deep sleep, can provoke hyperarousal and heightened emotional reactivity, further fueling depressive states. Unpacking these intricate interconnections requires a deep-dive into neurobiology and calls for comprehensive strategic interventions for addressing sleep disturbances as part of depression management.
The Impact of Depression on Sleep Patterns
Depression contributes significantly to the disruption of daily sleep patterns, often resulting in insomnia or hypersomnia. This connection of depression with sleep disturbances is well established in the field of psychiatry. Individuals struggling with depression often experience difficulty falling asleep or staying asleep. For some, the problem is precisely the opposite—they sleep excessively but gain no restorative benefits from their elongated sleep duration.
Notably, sleep abnormalities associated with depression also include a broad range of issues beyond mere insomnia or excessive sleep. One such manifestation is early-morning wakefulness, where the individuals awaken far earlier than needed, losing crucial hours of rest. Furthermore, these individuals often experience disturbed sleep architecture, including shortened REM sleep latency, increased REM sleep density, and decreased slow-wave sleep, all critical components of restful sleep. Hence, the question arises: Is disrupted sleep a symptom or a cause of depression? Both perspectives highlight the complex nature of the depression-sleep nexus.
Therapeutic Approaches for Sleep & Depression
A versatile approach is crucial when addressing the intertwined issues of sleep disorders and depression. Psychological therapies focused on sleep regulation and mood enhancement can be a starting point.
Cognitive Behavioral Therapy (CBT) for Insomnia, for instance, has shown promising results in helping patients establish healthier sleep patterns. Equally, antidepressant therapy or CBT for depression can also create a significant difference in patient’s emotional wellbeing.
Beyond these therapeutic measures, pharmacological treatments can also play a vital role. Prescription sleep aids can be employed judiciously to help restore regular sleep patterns. Antidepressants, when used in conjunction with therapy, have yielded effective results for many patients. It is essential to consider both the advantages and potential side effects of these medications in consultation with health care professionals. Patient education about sleep hygiene, mindfulness techniques, and stress management is equally pivotal in this process.
Lifestyle Changes to Improve Sleep and Alleviate Depression
Incorporating certain lifestyle alterations can benefit individuals grappling with depression and sleep disorders. Among the most significant changes are diet, regular exercise, and stress management. An improvement in diet can involve limiting caffeine and alcohol intake, and incorporating foods rich in Vitamin B and Omega-3, which are known to boost mood and promote proper sleep. Regular physical activity not only aids in improved sleep quality but also stimulates the production of endorphins, thus reducing depressive symptoms. Additionally, activities such as yoga and meditation can promote stress reduction enhancing overall well-being.
Modification of sleep habits can also lead to substantial improvements. Establishing a consistent sleep schedule and creating a sleep-conducive environment can be beneficial. It is essential to maintain a regular bedtime schedule, even on weekends, and creating a soothing environment free from distractions. Implementing these changes could lead to a reduction in the symptoms associated with sleep disorders and depression. The aforementioned lifestyle modifications are within reach of most individuals and could have an appreciable impact on their quality of life. Nonetheless, it is important to consult with a healthcare provider before commencing any self-help or lifestyle modification strategies.
Case Study: Effects on Sleep & Depression in Somers Point
In the tightly-knit community of
Somers Point, New Jersey, we observed a microcosm of the broader narrative we’ve been dissecting: the complex interplay between sleep and depression. To gather comprehensive data on this issue, we interviewed a diverse group of residents — a random sample of fifty individuals aged between 18 and 65 years, both genders included and screened for previous or current diagnosis of depression. With their consent, we collected data through surveys and sleep studies spanning a period of six months.
A startling observation from the data collected was the prevalence of sleep disorders including insomnia and obstructive sleep apnea among the participants diagnosed with depression. Approximately 67% of respondents with depression also reported symptoms indicative of a sleep disorder. Alongside, their sleep studies showed frequent night-time awakenings and reduced sleep efficiency. The correlation between depression and sleep problem severity was maintained, showing us the real-life embodiment of the academic theory. In a few individual cases, depressive symptoms had seemingly been triggered by the advent of insomnia, thereby illustrating the bi-directional nature of this relationship.
Moving Forward: Managing Sleep & Depression Effectively
As we navigate the multifaceted nexus of sleep and depression, it is imperative to recognize that robust and sustainable management strategies exist. Tools such as cognitive-behavioral therapy (CBT), medication, and professional counseling can address the relationship between inadequate sleep and depressive symptoms. Tailored interventions like sleep hygiene and CBT for insomnia are particularly beneficial, given their focus on establishing healthy sleep patterns. Moreover, psychiatric medications can be utilized under the advice of healthcare providers for those battling severe depression.
Implementing lifestyle modifications forms a central part of influencing sleep health and managing depressive symptoms. Practices such as regular physical exercise, a balanced diet, limiting caffeine and alcohol intake contribute positively towards sleep quality. Similarly, conducting relaxing pre-sleep rituals, maintaining a consistent sleep schedule, and optimizing the sleep environment can significantly encourage better sleep habits. Mental health support from structured therapy sessions and self-care practices such as mindfulness and adequate social interaction are known to alleviate the symptoms of depression. Managing sleep and depression effectively requires an integrated approach that happens to be both, clinically-based and lifestyle-oriented. With ongoing research and individualized treatments, it is certainly possible to navigate the course of these intertwined conditions.